Understanding the Hidden Story of a Heart Attack: A simple Guide to Myocardial Infarction
Title: Understanding the Hidden Story of a Heart Attack: A simple Guide to Myocardial Infarction
Introduction:
When it comes to matters of the heart, it's not just about love and emotions—it's also about the intricate dance of biology that keeps this vital organ ticking. One significant event that can disrupt this rhythm is a myocardial infarction, commonly known as a heart attack. In this article, we'll take a stroll through the pathophysiology of a heart attack, unraveling the mystery behind this potentially life-changing event. To guide us on this journey, we'll occasionally tap into the expertise of Dr. Olechowski, a private cardiologist with a wealth of experience, who often sees patients in Winchester at Sarum Road Hospital and at Candover in Basingstoke.
Main Text:
Imagine your heart as a powerful pump, tirelessly working to circulate blood throughout your body. This blood carries essential oxygen and nutrients, ensuring that every cell receives the sustenance it needs. However, just like any intricate machine, the heart can face malfunctions, and one such malfunction is a myocardial infarction.
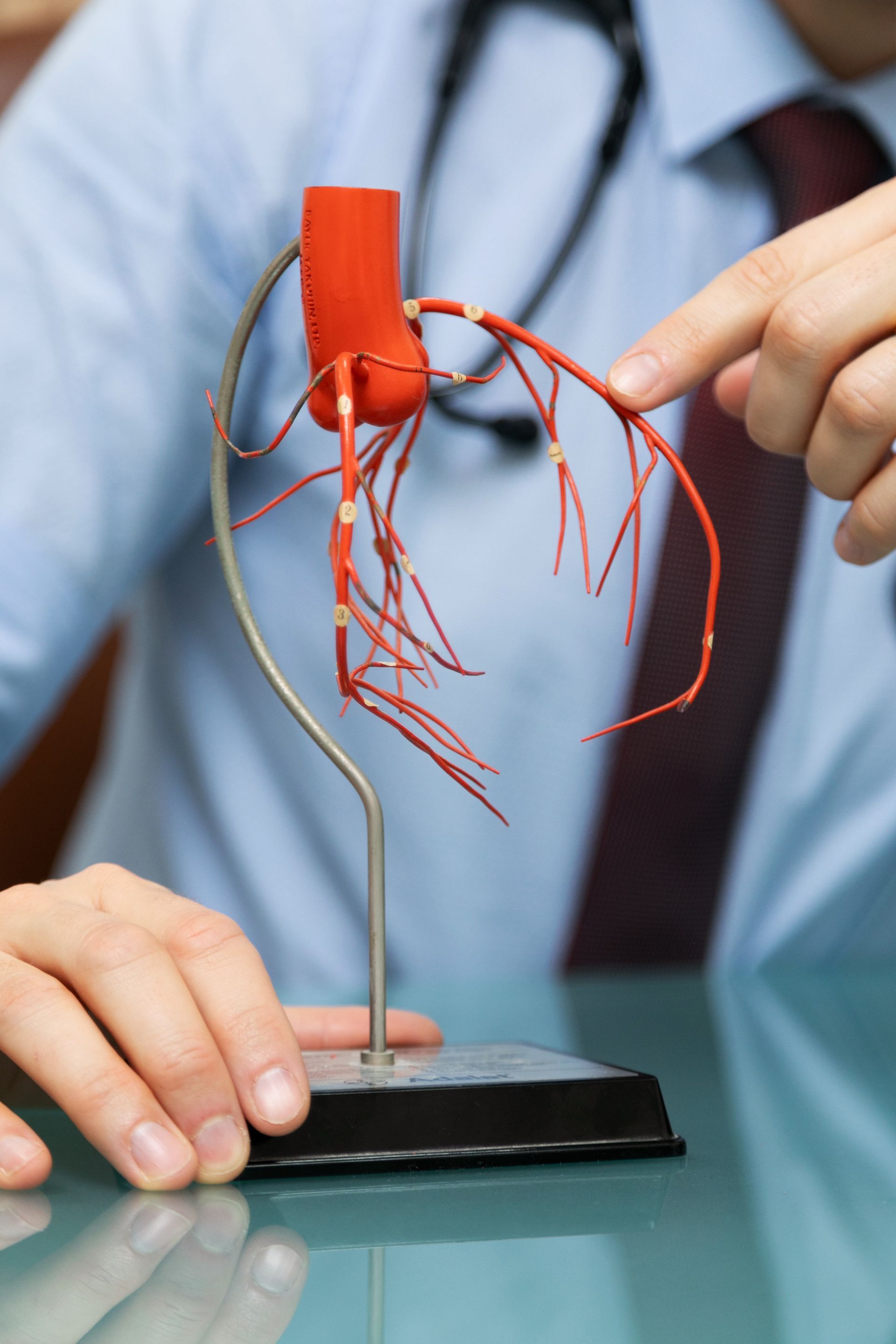
At the core of a heart attack lies a blocked coronary artery. These arteries are the highways that deliver oxygen-rich blood to the heart muscle. When one of these arteries becomes obstructed, it's like a roadblock preventing the flow of traffic. The culprit behind this blockade is often a blood clot, which forms at the site of a ruptured cholesterol plaque.
To understand this, think of your arteries as pipelines transporting blood. Over time, these pipelines can develop deposits, much like the gunk that accumulates in a clogged drain. These deposits, composed of cholesterol and other substances, can rupture, triggering a series of events that lead to clot formation.
As the clot grows, it can completely block the artery, cutting off the oxygen supply to a portion of the heart muscle. This is where the term "infarction" comes into play, indicating tissue death due to lack of blood flow. The affected part of the heart is deprived of oxygen, and if blood flow isn't restored promptly, permanent damage can occur.
Dr Olechowski sheds light on the urgency of recognizing the symptoms. "Time is of the essence when it comes to a heart attack. If you experience chest pain, shortness of breath, or discomfort in your upper body, seeking medical attention promptly can make all the difference."
In response to the reduced blood flow, the heart muscle may start to release certain enzymes into the bloodstream. These enzymes, such as troponin, serve as biochemical markers of heart muscle damage. Cardiologists like Dr Bart use these markers to assess the extent of injury and formulate a treatment plan tailored to the patient's needs.
Conclusions:
Understanding the pathophysiology of a myocardial infarction is like deciphering a complex narrative written in the language of the heart. As we've explored, a heart attack is not a sudden, random event; it's a consequence of a series of events that unfold in the cardiovascular system. Recognizing the signs and seeking prompt medical attention can be the turning point between a full recovery and lasting damage.
Dr Olechowski emphasizes the importance of proactive heart health. "Prevention is key. Regular check-ups, a healthy lifestyle, and managing risk factors like high blood pressure and cholesterol can significantly reduce the likelihood of a heart attack."
===============================================================
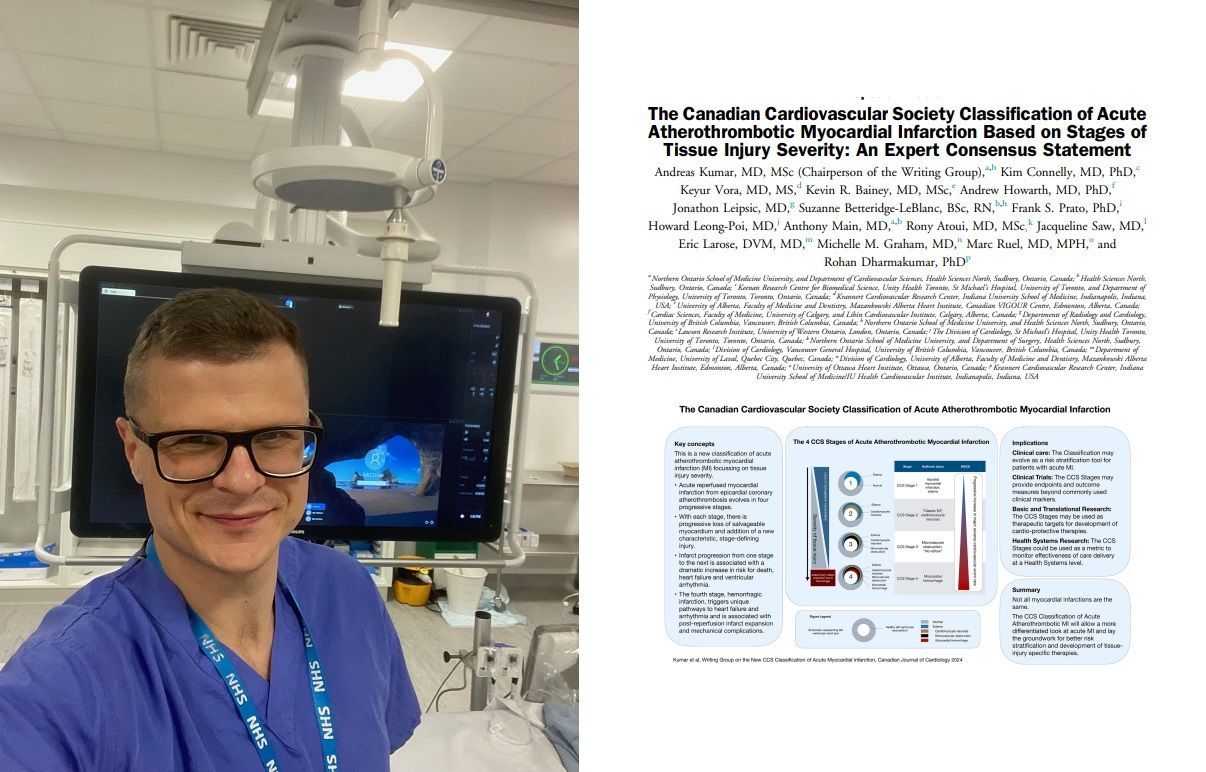
For medical professionals only, there are now Four STAGES of an Acute Heart Attack, which are described in the article above, according to the Canadian Cardiovascular Society (CCS), which also classified Angina in the past into 3 categories.
Stage 1: Aborted Myocardial Infarction (zero or minimal myocardial necrosis 'death of heart cells').
Stage 2: Myocardial infarction with significant cardiomyocyte necrosis but without microvascular injury.
Stage 3: So called 'No-reflow', death of heart muscle cells and microvascular obstruction. Every interventionist knows what 'no reflow' means and how difficult it is to treat it.
Stage 4: Death of heart cells and microvascular necrosis causing secondary reperfusion haemorrhage.
Link to full article below ⬇️:
https://onlinecjc.ca/article/S0828-282X(23)01735-X/fulltext
Hopefully this classification and recognising patients in particular category will lead to more targeted, individualised therapy.
-----------------------------------------------
📸 taken during cath lab session in Basingstoke.